The field of regenerative medicine is witnessing groundbreaking advancements, with personalized lung transplants emerging as a promising solution for patients suffering from severe respiratory disorders. Chronic obstructive pulmonary disease (COPD) and pulmonary fibrosis are debilitating conditions that significantly impair lung function and quality of life. Traditional treatments often fall short, and the availability of donor lungs for transplants is limited. However, the development of custom lungs using a patient’s own cells offers a transformative approach to treating these conditions, potentially restoring respiratory function and improving survival rates.
The Burden of Severe Respiratory Disorders
Respiratory disorders such as COPD and pulmonary fibrosis are major health concerns globally, including in India. COPD, characterized by chronic bronchitis and emphysema, leads to progressive breathing difficulties, frequent hospitalizations, and a substantial decline in life quality. Pulmonary fibrosis, marked by the thickening and scarring of lung tissue, causes severe breathlessness and hypoxia. Both conditions have limited treatment options, often relying on symptom management and oxygen therapy. For advanced cases, lung transplantation remains the only viable option, but the scarcity of donor organs poses a significant barrier.
Personalized Lung Transplants: A Game-Changer
Personalized lung transplants involve creating custom lungs using the patient’s cells, specifically their stem cells. This innovative approach leverages bioprinting and tissue engineering technologies to develop lungs that are biologically compatible with the patient, thereby minimizing the risk of immune rejection and the need for immunosuppressive drugs. Here’s how this transformative process works:
- Cell Harvesting and Cultivation:
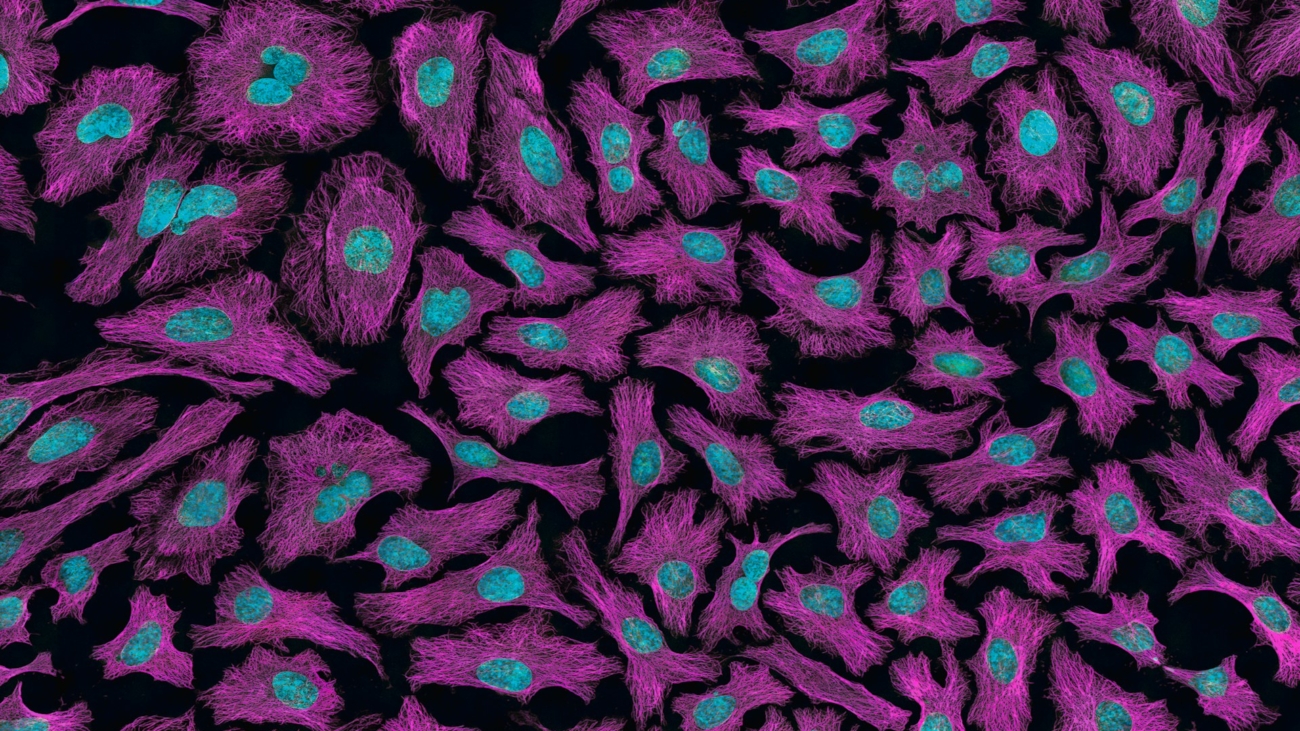
- The process begins with harvesting stem cells from the patient’s body, typically from bone marrow or adipose tissue. These cells are then cultivated and differentiated into lung-specific cells in a controlled laboratory environment.
- Bioprinting and Scaffold Creation:
- Using advanced 3D bioprinting technology, a scaffold that mimics the complex structure of the lung is created. This scaffold serves as a framework for the lung cells to grow and organize into functional lung tissue. The bioprinter precisely layers the cells and biomaterials to replicate the intricate architecture of the lung, including airways and blood vessels.
- Tissue Maturation and Integration:
- The bioprinted lung scaffold is placed in a bioreactor that provides optimal conditions for tissue maturation. Over time, the cells proliferate and integrate, forming a fully functional lung. This maturation process ensures that the lung is capable of performing essential respiratory functions, such as gas exchange.
- Transplantation and Recovery:
- Once the custom lung is fully developed and tested for functionality, it is transplanted into the patient. Since the lung is created from the patient’s own cells, the risk of immune rejection is significantly reduced. Post-transplant, the patient undergoes rehabilitation and monitoring to ensure successful integration and recovery.
Benefits of Personalized Lung Transplants
1. Reduced Risk of Rejection
- Traditional lung transplants often require lifelong immunosuppressive therapy to prevent organ rejection, which can lead to serious side effects and complications. Personalized lung transplants, created from the patient’s cells, are inherently compatible with the recipient’s immune system, drastically reducing the likelihood of rejection and the need for immunosuppressive drugs.
2. Increased Availability
- The shortage of donor lungs is a critical issue in the current transplant paradigm. By using a patient’s cells to create custom lungs, the dependence on donor organs is eliminated, making lung transplants more accessible to those in need.
3. Improved Survival Rates
- Personalized lung transplants can potentially offer better long-term outcomes compared to traditional transplants. The custom lungs are tailored to the patient’s specific biological requirements, enhancing the chances of successful integration and function.
4. Enhanced Quality of Life
- For patients with severe respiratory disorders, personalized lung transplants can significantly improve their quality of life. Restored lung function allows for greater physical activity, reduced symptoms, and fewer hospitalizations, enabling patients to lead more active and fulfilling lives.
The Future of Respiratory Care
While personalized lung transplants are still in the experimental stages, the progress in this field is promising. Clinical trials and continued research are essential to refine the techniques and ensure safety and efficacy. As technology advances, the potential for widespread application of personalized lung transplants becomes increasingly feasible.
In India, where respiratory disorders pose a significant health burden, embracing such innovative solutions could revolutionize respiratory care. Collaborative efforts between researchers, healthcare providers, and policymakers are crucial to advancing this technology and making it accessible to patients.
Conclusion
Personalized lung transplants represent a beacon of hope for patients suffering from severe respiratory disorders like COPD and pulmonary fibrosis. By leveraging the power of bioprinting and tissue engineering, this innovative approach offers a path to restoring respiratory function and improving survival rates. As research and technology continue to evolve, personalized lung transplants could become a cornerstone of respiratory care, transforming the lives of countless patients and redefining the future of transplant medicine.